Ambulatory care has become an increasingly important aspect of healthcare delivery, with more patients seeking care outside of traditional hospital settings. As such, enhancing ambulatory care practices and innovations is crucial for improving patient outcomes, streamlining healthcare delivery, and reducing costs. This article will explore some of the best practices and innovations in ambulatory care that have emerged in recent years.
One notable area of focus in enhancing ambulatory care is leveraging technology to improve outcomes. Advances in telemedicine and remote monitoring technologies have allowed providers to offer virtual consultations and remotely monitor patients’ vital signs from afar. These technologies not only increase access to care but also enable earlier intervention when health issues arise, ultimately leading to improved patient outcomes. Additionally, the use of electronic medical records (EMRs) has enabled providers to better track patient data over time, identify patterns or potential chronic conditions early on, and develop personalized treatment plans. By incorporating technology into their practice models, providers can enhance the quality of ambulatory care while simultaneously lowering costs for both patients and healthcare systems alike.
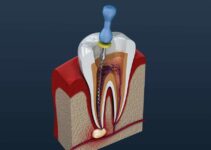
Leveraging Technology for Improved Outcomes

Source: inovalon.com
The utilization of technology has become a crucial factor in improving outcomes within the ambulatory care setting. Smart devices have revolutionized healthcare by enabling patients to monitor their health status at home and share this data with healthcare providers. For instance, wearable sensors can track vital signs like heart rate, blood pressure, and glucose levels, allowing physicians to detect early warning signs and intervene promptly. Moreover, smart devices can provide patients with reminders for medication adherence or follow-up appointments, reducing the risk of missed appointments or delayed treatment.
Telemedicine solutions have also emerged as an essential tool for enhancing ambulatory care outcomes. These technologies enable remote consultations between patients and healthcare providers through videoconferencing or phone calls. Telemedicine offers several benefits such as increased access to care for rural or underserved populations, reduced travel time and costs for patients, improved patient satisfaction, and better coordination of care among multiple providers. Furthermore, telemedicine can help prevent unnecessary emergency department visits or hospitalizations by providing timely interventions for acute conditions before they worsen. To find a telemedicine website for enhancing ambulatory care, you can conduct a search using keywords such as “telemedicine for enhancing ambulatory care” or “online healthcare services for outpatient care” on popular search engines. Additionally, you can reach out to local healthcare providers and inquire if they offer telemedicine services specifically aimed at enhancing ambulatory care.
In conclusion, leveraging technology in ambulatory care settings holds great promise for improving patient outcomes through smarter monitoring and more efficient delivery of care.
Redefining the Patient Care Experience
Redefining the patient care experience involves implementing strategies that prioritize patient-centered care, such as increasing patient engagement and improving communication between patients and healthcare providers. One way to achieve this is through virtual consultations, which allow for convenient access to healthcare services and improved communication between patients and their providers. Virtual consultations also provide an opportunity for personalized care plans that take into account a patient’s unique needs, preferences, and circumstances.
Personalized care plans can improve health outcomes by tailoring treatment options based on a patient’s individual factors, such as genetics, lifestyle habits, and medical history. This approach not only improves the quality of patient care but also reduces healthcare costs by avoiding unnecessary interventions or treatments. Overall, redefining the patient care experience through virtual consultations and personalized care plans can lead to improved health outcomes and greater patient satisfaction in the ambulatory setting.
Streamlining Healthcare Delivery
Source: technology-innovators.com
Streamlining healthcare delivery involves optimizing processes and systems to increase efficiency, reduce wait times, and improve access to care. Process optimization is an essential component of streamlining healthcare delivery as it ensures that resources are used effectively. By analyzing the current processes in place, healthcare providers can identify areas of improvement and develop strategies to make them more efficient. This approach can help eliminate redundancies in workflows, reduce administrative tasks, and automate routine procedures.
Resource allocation is another critical aspect of streamlining healthcare delivery. Ensuring that resources such as staff, equipment, and supplies are allocated appropriately can help reduce wait times for patients while improving their overall experience. With proper resource allocation, patients receive timely care from trained professionals equipped with the necessary tools to provide high-quality services. Additionally, streamlining resource allocation can lead to cost savings by reducing waste and ensuring that all resources are used optimally. In conclusion, process optimization and resource allocation are key strategies for enhancing ambulatory care by streamlining healthcare delivery processes. These approaches can lead to increased efficiency, improved patient outcomes and experiences while also reducing costs for both patients and providers alike.
Patient Engagement and Empowerment
Patient engagement and empowerment can be likened to a spark that ignites a fire of positive change in healthcare, as it actively involves patients in their own care and decision-making processes. This approach is all about placing the patient at the center of the healthcare experience, empowering them with knowledge, and involving them in conversations about their health goals. Patient education plays a crucial role in this process, as it helps individuals understand their health conditions better and make informed decisions about their care.
Effective communication strategies are also key to patient engagement and empowerment. Healthcare providers must ensure that patients have access to clear information about their health status, treatment options, and potential outcomes. They must listen actively to patients’ concerns and questions, provide answers in plain language, and encourage dialogue throughout the care process. By implementing these strategies, healthcare providers can help patients take an active role in managing their health while fostering trust between themselves and those they serve. Ultimately, patient engagement and empowerment can lead to better outcomes for both patients and providers alike.
Utilizing Data Analytics for Enhanced Care

Source: actian.com
Utilizing data analytics in healthcare has become increasingly important in improving the quality of care and patient outcomes. Predictive modeling, for instance, has been gaining traction as a tool to identify patients who are at risk of developing certain diseases or conditions even before symptoms manifest. This enables healthcare providers to intervene early on and provide personalized interventions that can mitigate the progression of such conditions. For example, predictive analytics can help identify patients with diabetes who are likely to develop complications such as diabetic retinopathy or kidney disease. By providing these patients with personalized interventions like regular eye exams or medication adjustments, healthcare providers can prevent the onset or exacerbation of these complications.
Aside from improving patient outcomes, utilizing data analytics in healthcare also offers benefits for providers and payers alike. By identifying high-risk patients early on and intervening before their conditions worsen, provider organizations can reduce hospital readmissions and lower costs associated with caring for sicker patients. Payers also benefit from improved patient outcomes because it reduces the overall cost of care over time. As such, utilizing data analytics is an effective way to improve not just individual patient outcomes but also the overall health system’s performance by reducing costs while simultaneously enhancing care quality and efficiency through personalized interventions based on predictive modeling results.
Collaborative Care Models and Interdisciplinary Teams
Collaborative care models and interdisciplinary teams have become increasingly popular in healthcare, like a symphony orchestra where each member plays a unique role to create a harmonious whole. The patient centered approach is at the core of this model, as it involves not only the physician but also other healthcare professionals working together to provide comprehensive care that meets the needs and preferences of the patient. Interdisciplinary teams are composed of various specialists including nurses, social workers, pharmacists and physical therapists who collaborate with physicians to develop individualized treatment plans that take into consideration all aspects of a patient’s health.
One key element of collaborative care models is shared decision making. This means that patients are actively involved in their own care by participating in discussions about treatment options and making informed choices based on their values and goals. Shared decision making has been shown to improve outcomes for patients while reducing healthcare costs by avoiding unnecessary treatments or procedures. Overall, collaborative care models and interdisciplinary teams represent an important shift towards more patient-centered care that prioritizes teamwork and communication among healthcare professionals.